The Role of Predictive Analytics in Combating Hospital-Acquired Infections (HAIs)

Introduction: A Quiet Crisis in Health Care
Addressing hospital-acquired infections (HAIs) has become one of the biggest challenges in contemporary healthcare. Although medical technology and hygiene protocols have improved greatly, healthcare-associated infections (HAIs) still affect millions of patients globally each year, causing longer hospital stays, higher treatment costs, and increased mortality rates. Multidrug-resistant pathogens also complicate the picture, leading to infections that cannot be treated easily.
Current infection control practices are reactionary—contagions are typically discovered only after an outbreak is underway. But in the age of data, predictive analytics is proving to be a useful ally in the fight against HAIs before they take hold. Predictive analytics is changing the infection control landscape by turning to real-time data, ML models, and AI-assisted insights, shifting prevention from a reactive stance to proactive intervention, helping hospitals and other healthcare settings get ahead of spreading cases.
Infections Acquired in a Hospital
These are infections that patients acquire while in a healthcare facility and were not present at the time of admission. Common HAIs include:
– Ventilator-associated pneumonia (VAP)
– Catheter-associated urinary tract infections (CAUTI)
– Surgical site infections (SSI)
– Bloodstream infections (BSI)
– Clostridium difficile (C. diff) infections
These infections are commonly caused by bacteria, viruses, and fungi and are often exacerbated by prolonged hospital stays, surgical interventions, antibiotic misuse, and inadequate hand hygiene.
Infection control policies are already rigorous, yet human error, environmental factors, and the lack of surveillance capabilities continue to make HAIs an ongoing problem. This is where predictive analytics can be transformational.
Predictive Analytics: A Game-Changer in HAI Prevention
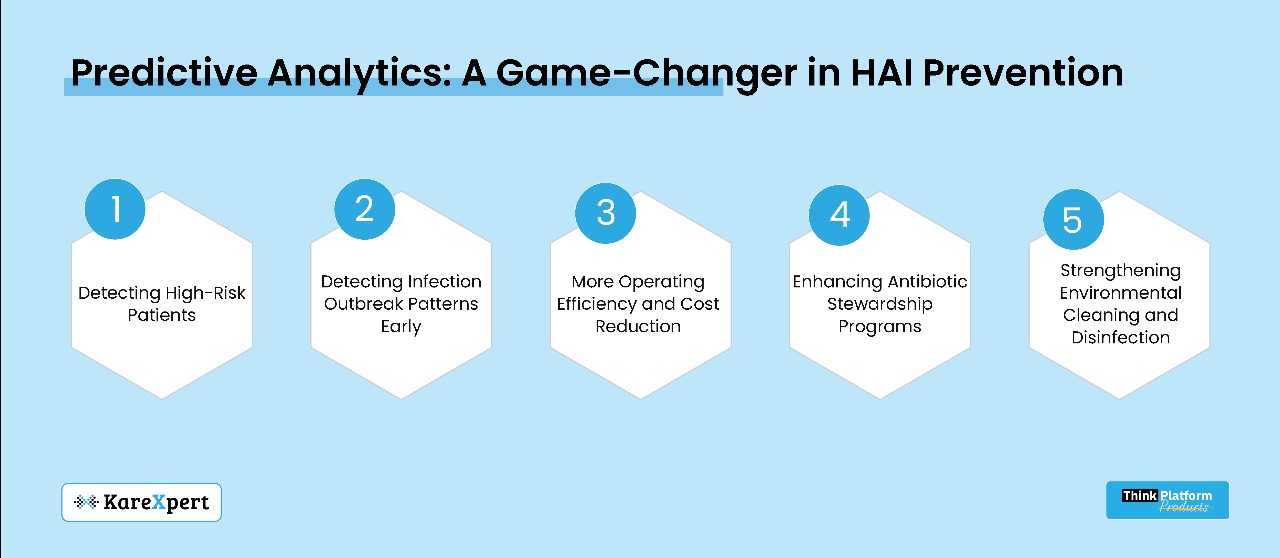
Predictive analytics uses data models to forecast infection risks, enabling healthcare providers to take proactive measures before an outbreak occurs. Here’s how it works:
1. Detecting High-Risk Patients
Patients are not uniformly at risk for HAIs. Predictive models analyze patient history, comorbidities, length of stay, medication usage, and prior infections to identify high-risk individuals. Flagging these patients early allows hospitals to apply tight monitoring, specific hygiene steps, and individualized preventive protocols.
For example:
– A diabetic patient with a weakened immune system hospitalized for surgery can be identified as high risk for surgical site infections.
– A ventilated patient in the ICU can be flagged as at risk for ventilator-associated pneumonia.
This allows hospitals to prioritize interventions based on real-time risk scoring.
2. Detecting Infection Outbreak Patterns Early
Outbreaks in hospitals are often detected after multiple patients have already been infected. Predictive analytics can help prevent this by flagging signals ahead of time, such as:
– Irregular surges of infections in a given ward.
– Clusters of similar infections occurring in rapid succession.
– Patterns of antibiotic resistance indicating a new superbug strain.
By integrating electronic health records (EHRs), microbiology laboratory data, and environmental surveillance, predictive analytics can preemptively alert infection control teams before outbreaks spiral out of control.
3. Monitoring Hand Hygiene Compliance
Proper hand hygiene is one of the simplest yet most effective ways to prevent HAIs. However, compliance rates among healthcare workers often fall short. Predictive analytics can:
– Analyze live hand hygiene data from IoT-connected sensors.
– Track non-compliance trends per shift, department, or individual.
– Automate alerts for infection control teams when hygiene lapses are detected.
For example, if the system identifies lower handwashing compliance rates among ICU nurses during night shifts, it can automatically implement targeted interventions (e.g., reminders, retraining, policy reinforcement).
4. Enhancing Antibiotic Stewardship Programs
Overuse and misuse of antibiotics contribute to antibiotic-resistant HAIs. Predictive analytics helps hospitals by:
– Analyzing prescription patterns to identify overuse trends.
– Adjusting treatment protocols based on real-time resistance patterns.
– Ensuring appropriate antibiotic selection to minimize resistance development.
By reducing unnecessary antibiotic exposure, predictive analytics lowers the likelihood of multidrug-resistant pathogens spreading within hospitals.
5. Strengthening Environmental Cleaning and Disinfection
Environmental contamination significantly contributes to HAI transmission. Predictive analytics can:
– Use environmental sensors to track pathogen hotspots in real-time.
– Identify high-touch surfaces (e.g., bed rails, IV stands, doorknobs) requiring frequent disinfection.
– Optimize cleaning schedules based on patient flow and infection risk data.
For instance, a machine learning model analyzing hospital foot traffic might determine that high-traffic wards require more frequent disinfection, reducing cross-contamination risks.
Case Studies: Predictive Analytics in HAI Control
Many hospitals worldwide are already leveraging predictive analytics to combat HAIs. Some notable examples include:
– Johns Hopkins Hospital developed a predictive calculator that scans patient data to flag individuals at risk for bloodstream infections up to 48 hours before symptoms appear.
– Cleveland Clinic uses AI-powered surveillance to monitor ICU patients for early signs of sepsis, enabling early intervention.
– The UK’s NHS employs real-time process analytics to track antibiotic-resistant bacteria and prevent outbreaks in high-risk units.
Predictive analytics is no longer just a theoretical concept—it is actively saving lives by enhancing infection prevention strategies.
Challenges and Considerations in Predictive Analytics for HAI Prevention
While promising, several challenges must be addressed for predictive analytics to be effectively implemented in infection control programs:
1. Data Integration Across Diverse Systems
Many hospitals use different IT systems, making it difficult to consolidate patient data, microbiology results, and infection control reports into a single predictive model.
Solution: Implement interoperable health information management systems (HIMS) that integrate data streams.
2. Transparency and Trust in AI Algorithms
Healthcare providers may hesitate to rely on AI-powered risk predictions if they do not understand how the models generate risk scores.
Solution: Use explainable AI models that provide actionable insights rather than opaque risk scores.
3. Balancing Automation with Human Expertise
Predictive analytics should supplement, not replace, human infection control experts. Over-reliance on algorithms without human validation may result in false alarms or missed infections.
Solution: Maintain a hybrid approach where clinicians validate AI-generated insights before implementation.
4. Privacy and Data Security Concerns
Patient privacy is a major concern in predictive analytics, particularly regarding data security and regulatory compliance.
Solution: Ensure compliance with healthcare data privacy laws and implement robust cybersecurity measures.
Future Outlook: AI-Driven Infection Control
The future of predictive analytics in infection control is promising, with advancements such as:
– Genomic sequencing to monitor bacterial evolution and anticipate resistance patterns.
– Biosensors that track patient physiology to detect early infection signs.
– AI-powered automated disinfection systems that adjust cleaning schedules based on real-time risk assessments.
By preventing the spread of HAIs, hospitals can take a significant step toward achieving zero preventable infections, safeguarding both patients and healthcare workers.
Summary: The Future of HAI Prevention is Predictive
Hospital-acquired infections pose a major global health risk, but predictive analytics is transforming infection control. By identifying high-risk patients, tracking hygiene compliance, optimizing antibiotic use, and preventing outbreaks before they occur, predictive analytics helps hospitals shift from reactive crisis management to proactive prevention.
Implementing predictive analytics in infection control strategies leads to lower infection rates, reduced costs, better patient outcomes, and an overall improvement in care quality. In the modern era of healthcare, proactive HAI prevention is critical, and predictive modeling may be the key to enhancing hospital safety in the future.
