The Psychology of Healing: Why Empathy is the Most Powerful Treatment Tool

We Are All Human, Whatever We Do and Wherever We Live
When we think of healing, we often consider the latest treatments, breakthrough drugs, and life-saving operations. However, the most undervalued and arguably most potent ingredient in healthcare isn’t found in a prescription or an operating room—it’s empathy.
For decades, modern medicine has prioritized efficiency, technological advancement, and precision-based treatments. Yet, increasing evidence shows that a patient’s emotional and psychological state can directly impact the success of treatment, recovery time, and overall well-being. Research demonstrates that patients who feel understood, cared for, and emotionally supported experience lower stress levels, stronger immune function, and faster recovery rates.
So if empathy is so powerful, why isn’t it a keystone of modern healthcare? Why do hospitals and doctors still operate within impersonal systems that treat patients as cases rather than people? More importantly, how can hospitals, healthcare professionals, and institutions incorporate empathy into their care models?
This article explores why empathy is one of the most important yet overlooked aspects of healthcare, how it actively affects patient outcomes, and what can be done to ensure empathy becomes an intrinsic part of every medical practice.
How Empathy and Healing Work, Scientifically
Although many people view empathy as an emotional or philosophical concept, there is substantial scientific evidence supporting its beneficial effects on physical and mental health.
1. How Compassion Activates the Body’s Self-Regeneration Processes
Empathy is not just about kind words or gestures—it has a biological impact on the body. When a patient feels authentic compassion and understanding from a doctor, their brain releases:
– Oxytocin: Often called the “bonding hormone,” oxytocin encourages relaxation, lowers stress levels, and fosters trust between patients, families, and caregivers.
– Endorphins: These natural painkillers reduce the perception of pain and promote an overall improved mood.
– Serotonin & Dopamine: These neurochemicals are vital for mood stabilization and motivation, both of which are crucial for patients dealing with chronic conditions or long-term treatments.
When a doctor takes the time to listen, acknowledges pain, and speaks with warmth and attention, the neurochemical responses help accelerate healing and improve adherence to treatment.
2. The Placebo Effect: Evidence That Belief and Trust Matter
The placebo effect—where a patient experiences real symptom relief after receiving a non-active treatment—is one of the most well-documented psychological phenomena in medicine.
What drives this effect? Trust and belief.
If a patient believes they are receiving the right treatment—especially when their doctor exudes confidence and empathy—their body responds positively.
A Harvard study found that placebo treatments given by doctors with warm, empathetic interactions produced greater pain relief and symptom reduction than the same placebos given in a neutral or rushed setting.
This is not just a “soft skill” but a proven factor in medical outcomes.
Why There Is So Little Empathy in Healthcare
If empathy is so strongly supported by science, why is it so often absent in healthcare?
1. Physician Burnout & Time Constraints
– The healthcare system is designed for efficiency, not emotional engagement.
– Doctors must see dozens of patients daily, leaving little time for meaningful interaction.
– Administrative work and electronic documentation take up valuable patient-facing time.
– Physician burnout is at an all-time high, making it difficult to emotionally connect with each patient.
2. Over-Reliance on Technology
– Electronic Health Records (EHRs), AI diagnostics, and telemedicine have improved efficiency but also increased the emotional distance between doctors and patients.
– Physicians spend more time looking at screens than at patients.
– Automated systems and chatbots, while helpful, have made the patient experience feel impersonal.
3. Traditional Medical Education Models
– Medical education prioritizes clinical knowledge, procedures, and diagnostics but not communication or emotional intelligence.
– Many doctors never receive formal training in active listening, bedside manner, or empathy-driven care.
– The medical culture often values efficiency over emotional support, discouraging doctors from taking extra time with patients.
If empathy is neither taught nor encouraged, how can it become a natural part of healthcare?
How Healthcare Can Make Empathy a Core Value
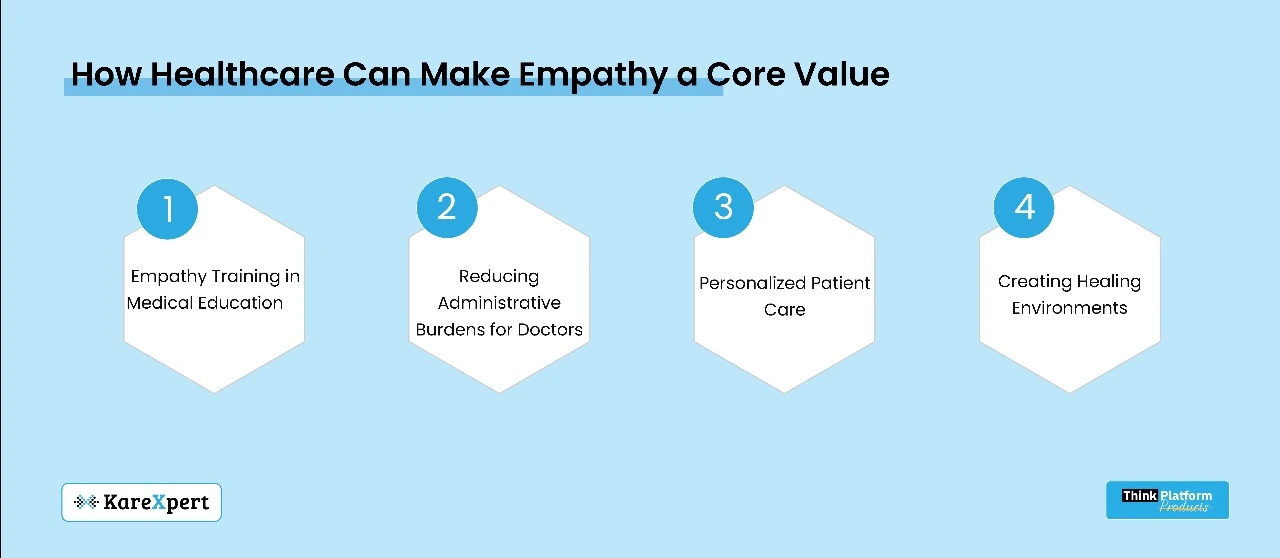
If we accept that empathy is critical to patient recovery, the next step is to incorporate it into medical practice. Here’s how:
1. Empathy Training in Medical Education
Medical schools and hospitals should prioritize empathy training so that future healthcare professionals can:
– Learn active listening techniques and patient-centered communication.
– Participate in simulated patient scenarios that develop emotional intelligence.
– Train in recognizing non-verbal cues of distress.
Hospitals that invest in empathy workshops and communication training see higher patient satisfaction and better health outcomes.
2. Reducing Administrative Burdens for Doctors
Hospitals can adopt AI-driven documentation tools, voice-to-text technology, and workflow automation to minimize paperwork, allowing doctors to spend more time interacting with patients.
3. Personalized Patient Care
Instead of treating patients as mere cases, healthcare providers should:
– Develop personalized care plans tailored to both medical and emotional needs.
– Check in compassionately throughout treatment—not just for medical updates.
– Follow up post-discharge to monitor both physical and emotional recovery.
4. Creating Healing Environments
A hospital’s physical environment plays a crucial role in emotional well-being. Hospitals can:
– Design waiting areas with natural lighting and soothing décor.
– Reduce noise pollution in patient rooms to lower stress levels.
– Implement video check-ins for family members to keep patients emotionally connected.
Conclusion: Empathy is the Future of Medicine
Healthcare is evolving. AI, robotic surgeries, and new medical innovations will shape the future of medicine, but one thing will never change: patients want to be treated as human beings, not numbers.
Empathy is not just a bonus in patient care—it is a core component of healing.
– Patients who feel heard and emotionally supported heal faster, experience less stress, and adhere to medical advice.
– When doctors and nurses prioritize human connection, they experience higher job satisfaction and lower burnout.
– Hospitals that embed compassion into their care models see higher patient trust, better recovery rates, and improved efficiency.
Medicine is both science and humanity. A simple act of understanding, a compassionate conversation, or a moment of human connection can do something no machine and no medicine can do: give a patient hope.
It’s time to reimagine healthcare—not just as a domain of cure but as a haven of healing, anchored in empathy.
