How Many Reports Are Lost Every Month? If You Don’t Know, You’re Already at Risk

In a hospital, no document is just a document. Every report, scan, prescription, and chart holds a piece of a patient’s health story. And when even one piece goes missing, the consequences ripple across care, operations, and even compliance. Yet, many healthcare institutions are surprisingly unaware of how many reports go untracked, misfiled, or simply vanish each month. If you’re not counting those losses, you may already be standing on a fault line.
The Silent Risk in the System
Unlike a system outage or a medical emergency, missing patient reports don’t always set off alarms. They hide in the background—until a clinician is forced to redo a test, a patient’s diagnosis is delayed, or worse, a legal issue arises because the document trail failed.
Hospitals that fail to monitor the integrity of their medical reporting ecosystem often discover too late that they have been bleeding data—and trust.
Three Kinds of Report Loss Most Hospitals Overlook
1. Transient Loss: A report exists but is temporarily inaccessible due to system delays, misplaced files, or outdated storage formats.
2. Operational Loss: A report is generated but never reaches the relevant department or clinician.
3. Permanent Loss: The report was never stored, was deleted unintentionally, or was saved to a system that is no longer retrievable.
Each type carries its own threat. The danger isn’t only the absence of data, but the erosion of operational reliability and patient safety.
Why Are Reports Still Going Missing?
Even in an age of digitized operations, the causes are more common than they should be:
– Legacy Systems with Limited Traceability: Systems that don’t have robust versioning, audit trails, or indexing mechanisms.
– Siloed Departments: Radiology might store data differently than pathology. And if one system doesn’t speak to the other, reports fall through.
– Manual Dependencies: When uploading or filing requires a human step, errors become inevitable.
– Temporary Workarounds: Temporary backups or external storage methods can turn into permanent problems.
When documentation and communication flows are not unified, it’s not just about inefficiency—it’s about exposure.
The High Cost of Invisible Loss
Lost reports aren’t just an operational hiccup. They leave behind real-world damage:
– Delayed Diagnoses: A missing radiology report may delay an oncology referral by weeks.
– Duplicated Tests: Patients are subjected to redundant procedures, increasing costs and reducing trust.
– Medicolegal Liability: Documentation gaps can leave hospitals vulnerable to litigation.
– Frustrated Staff: Clinicians waste time chasing reports rather than focusing on care.
– Broken Patient Trust: A patient who sees a provider flipping through missing pages is a patient who might not return.
Real Scenarios, Real Impact
At a mid-sized multi-specialty hospital, a missing blood panel report led to the delay of a surgical procedure. The patient’s condition worsened over 48 hours, and the family filed a grievance. Post-incident review showed that while the lab report had been generated, it was never uploaded due to a failed integration between lab equipment and the central system.
Another hospital in an urban metro area faced legal consequences when a prenatal scan was misplaced. The clinician operated on outdated assumptions, leading to a treatment misstep. The IT audit traced the issue to a naming mismatch in the system’s file directory.
But We Have a Digital System—Why Should We Worry?
Digital doesn’t automatically mean dependable. Most current hospital systems focus on data collection, not continuity. If a report exists in one format but isn’t traceable across systems, it’s as good as lost.
Modern hospitals need system-level redundancy that prevents reports from being:
– Unlinked
– Unsearchable
– Unsynchronized
And above all, they need real-time visibility into whether all reports are being delivered and read.
Are You Measuring What Matters?
Here’s a simple question: Can your hospital produce a real-time dashboard showing how many lab reports, scans, prescriptions, or discharge summaries were generated, reviewed, and acknowledged—today?
If you’re not measuring these metrics, you’re likely not managing the risk.
Metrics That Matter:
– Report Generation Time vs. Report Access Time
– Number of Reports Re-requested
– Average Time to Locate Archived Reports
– Percentage of Reports Delivered to the Wrong Department
– Number of Reports Pending Acknowledgment for Over 24 Hours
Without this data, you’re managing blind.
What a Better System Looks Like
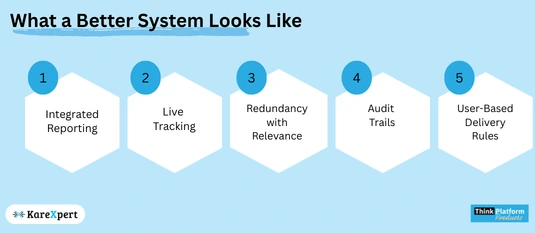
Hospitals need more than a reporting tool—they need an ecosystem.
A modern hospital information system should offer:
– Integrated Reporting: One interface that pulls from labs, radiology, OPD, and wards.
– Live Tracking: Know where every report is in its lifecycle.
– Redundancy with Relevance: Real-time backups and failovers that retain user context.
– Audit Trails: Every change, access, or delay is tracked.
– User-Based Delivery Rules: Reports get delivered based on clinician roles and relevance, not static hierarchies.
Beyond Compliance: Building a Culture of Accountability
This isn’t only about passing NABH or JCI audits. It’s about embedding reliability into the bloodstream of your hospital. When a radiologist knows their report will be instantly seen by a referring surgeon, they’re more invested in quality and speed. When IT can detect a report bottleneck in real time, it avoids chaos.
Accountability is not punitive—it’s preventive.
How to Start Fixing It Today
1. Conduct a Report Flow Audit: Map every report’s journey from generation to delivery.
2. Measure Current Loss: Track how many reprints or re-requests happen weekly.
3. Talk to Frontline Staff: Ask nurses and doctors where they lose time chasing data.
4. Eliminate Manual Handoffs: Automate wherever possible.
5. Implement Role-Based Access Dashboards: Know who has seen what, and when.
The Bottom Line
If your hospital doesn’t know how many reports go missing, you’re already at risk.
You can’t fix what you can’t track. And in healthcare, invisibility is not safety—it’s vulnerability.
Whether it’s the missed diagnosis that slipped through a paper crack or the revenue that vanished with a misfiled test, the cost of lost reports is more than financial. It’s reputational. It’s clinical. It’s human.
Don’t wait for a crisis. Start counting what matters.
Because in modern healthcare, what gets measured isn’t just managed—it’s safeguarded.
