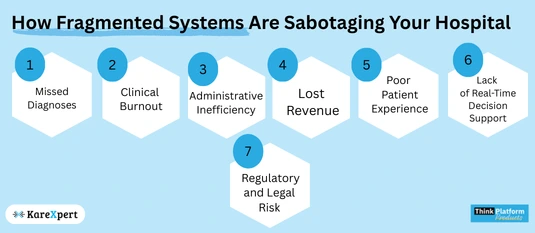
From Missed Diagnoses to Lost Revenue: How Fragmented Systems Are Sabotaging Your Hospital

Introduction: When Systems Fail, Patients and Profits Suffer
Hospitals today stand at a critical junction: the push for digital transformation has brought hundreds of tools, platforms, and vendors into the healthcare space, each promising solutions to individual problems. But what happens when these tools don’t talk to each other? What happens when your radiology department runs on one system, your billing another, and your outpatient clinic uses something else entirely? You get fragmentation—the silent saboteur.
This article explores how system fragmentation isn’t just an IT inconvenience but a clinical and financial liability. From diagnostic errors to revenue leaks, the cost of operating in silos is far greater than you might think.
1. Missed Diagnoses: When Information Gets Lost in Translation
Clinicians rely on the seamless flow of patient data to make accurate, timely decisions. But when diagnostic systems are disconnected from patient history, and when lab reports sit on a different platform than imaging results, you have a perfect storm for missed diagnoses.
Consider this scenario: A patient comes into the ER with chest pain. The EHR contains notes from a previous visit showing abnormal ECG readings, but the data resides in a different platform not visible to the ER physician. The result? Duplicate tests, misdiagnosis, and delayed care.
Clinical Fallout:
– Redundant or missed tests
– Incomplete patient history
– Increased diagnostic error
2. Clinical Burnout: The Human Cost of Digital Chaos
Fragmented systems don’t just affect patients; they wear down your most valuable asset—your staff. When clinicians need to toggle between five different platforms just to complete one patient round, it takes a toll.
Documentation becomes tedious. Time spent on patient interaction drops. Morale plummets. And burnout follows. In a landscape already stretched thin by workforce shortages, hospitals can’t afford to ignore the burden of tech inefficiency.
What staff are saying:
– “We spend more time documenting than treating.”
– “Each department speaks a different software language.”
– “Simple tasks feel like multi-step missions.”
3. Administrative Inefficiency: Duplicated Work, Delayed Processes
Let’s talk numbers. Administrative departments dealing with patient records, insurance claims, and billing often work across multiple incompatible systems. That means more manual entries, more room for human error, and more time spent reconciling data than using it.
When systems don’t sync:
– Billing gets delayed.
– Claims are denied due to missing documentation.
– Audits become nightmares.
If your admin team is spending more time pulling data from scattered platforms than actually optimizing operations, fragmentation is the root cause.
4. Lost Revenue: The Financial Black Hole
Healthcare margins are razor thin. Hospitals can’t afford inefficiencies that erode profitability, but that’s exactly what fragmented systems do. Revenue cycle leaks are often caused by breakdowns in data transmission across systems.
Revenue Leakage Points:
– Delayed discharge leading to longer bed occupancy
– Under-coding due to incomplete clinical documentation
– Missed charges because ancillary services weren’t captured
These are not minor slips; they amount to millions in lost revenue annually for mid- to large-sized hospitals.
5. Poor Patient Experience: Fragmentation Feels Like Indifference
Modern patients expect seamless experiences. They book appointments through mobile apps, track their fitness data, and expect the same digital fluency from their healthcare providers.
But when patients are asked to repeat the same information at every touchpoint or when follow-up reports don’t sync with their main profile, trust erodes. Fragmented systems translate into fragmented care.
Patient Experience Red Flags:
– Repeated form-filling and identity verification
– Inconsistent communication across departments
– Lack of transparency in billing or discharge process
6. Lack of Real-Time Decision Support
Healthcare decisions are time-sensitive. A lag in information can mean the difference between proactive treatment and medical escalation. Yet, most fragmented systems don’t offer real-time insights because data is scattered, delayed, or inaccessible at the point of care.
Without centralized dashboards or integrated analytics, clinical decisions are made on partial data, which is not only risky but also inefficient.
7. Regulatory and Legal Risk
Fragmented systems make regulatory compliance difficult. Whether it’s data protection regulations or audit requirements, the inability to maintain a consistent, complete trail of patient interactions can trigger legal consequences.
Hospitals risk:
– Fines for non-compliance
– Data breaches due to poor system integrations
– Failed audits or accreditation delays
A Unified System Is No Longer a Luxury—It’s Survival
Hospitals that continue to operate with disconnected systems are choosing to accept risk—clinical, financial, operational, and reputational. It is no longer about digital adoption; it is about digital unification.
Solutions that offer end-to-end integration of clinical, administrative, and diagnostic modules are proving to be not just efficient but transformative. These platforms bring together every stakeholder—from frontline clinicians to billing officers—under one interoperable ecosystem.
Real-World Impact: What Integration Can Solve
– ER physician sees full patient history in real-time.
– Lab reports auto-sync with EHRs, no manual uploads.
– Billing auto-generates from clinical documentation.
– Discharge summaries and prescriptions pushed to mobile apps.
– Admin dashboards reflect live bed occupancy and resource status.
This isn’t a tech wishlist—it’s what hospitals with unified systems are achieving today.
Final Thoughts: Stop Fixing, Start Transforming
If your hospital is constantly troubleshooting its own internal miscommunication, you’re not innovating—you’re firefighting. Fragmentation is not a minor issue. It’s a full-blown crisis in disguise. And unless addressed at the root level, it will continue to drag down clinical care, operational efficiency, and financial sustainability.
It’s time to stop patching old systems and start building new foundations. Because the future of healthcare won’t wait for departments to get on the same page—it demands they already are.
