From Ambulance to Admission: Why Emergency Departments are Failing in Speed and Efficiency

Introduction — A Race Against Time in Emergency Care
In the golden hour—the short time frame after a medical emergency that is the deciding factor in whether a patient recovers or goes into decline. However, despite advances in medical technology, emergency departments (EDs) worldwide face ongoing challenges with inefficiencies that lead to delays in care. From delayed handovers of patients between ambulances and emergency departments to congested triage systems, the very spaces designed to save lives are often plagued by systemic delays that impact patient outcomes.
This is how ambulance services are falling short in speed and efficiency, and how hospitals need to step up now to close the gap from ambulance arrival to patient admission — what we expose in this article.
Emergency Department Bottlenecks
1. The Ambulance Handover Crisis
Ambulance crews commonly have long turnaround times before they can transfer patients to emergency departments that are often unprepared to accept patients on arrival.
When ambulances are stranded outside hospitals, unable to discharge patients, it creates a backlog, preventing emergency responders from attending to new cases.
Many hospitals do not even have a system for real-time bed management, so there is no proactive allocation of spaces for incoming patients.
2. Outdated Triage Systems
Existing triage mechanisms depend significantly on manual evaluations, leading to bottlenecks at the very first point of care.
Without AI-driven decision support, overall assessments are often based on unstructured impressions, sometimes underestimating the gravity of the cases.
In the absence of real-time integration with hospital resources, ED personnel lack the data needed to prioritize admissions intelligently.
3. Staffing Shortages and Burnout
Overly strained emergency rooms cause delayed reactions, miscommunication, and patient dissatisfaction.
High-pressure environments can lead to burnout, increased turnover, and lower quality patient care.
Inadequate coordination among paramedics, triage nurses, and the attending physician causes delays in treatment.
4. Diagnostic Delays
One of the biggest reasons behind delays in emergency department care is when physicians have to wait for critical test results.
Separate, non-integrated diagnostic systems used by hospitals result in a breakdown of communication between labs and emergency departments.
Radiology and pathology workflows operate inefficiently, leading to increased wait times for critical diagnostics.
5. Failure to Track Bed Availability in Real-Time
Many hospitals rely on manual or outdated systems to track bed availability, which contributes to avoidable congestion in the ED.
When there is no automated discharge planning, patient flow slows, and at-risk patients are left without a bed.
The Key to Speed and Efficiency: Technology
1. AI-Enhanced Triage Systems
AI-powered triage effectively reduces waiting times in hospitals by analyzing patients based on reported symptoms and severity instantly.
Predictive analytics can provide accelerated prioritization to avoid overflow of low acuity patients in ED workflows.
AI-powered models help detect critical illnesses such as strokes, cardiac arrests, and sepsis with greater speed.
2. Resource and Patient Decision Tools in Automated Bed and Bedside Resource Allocation
By implementing real-time bed management systems that dynamically allocate beds, hospitals can minimize excessive waiting times.
Cloud-based HIMS has enabled seamless communication between ED, inpatient wards, and ICU.
Smart logistics can also improve the flow of patients from admission to treatment.
3. Coordinated Ambulance Services
GPS-enabled ambulance tracking allows hospitals to prepare before patients arrive.
Paramedics now share data in real time with teams at hospitals, enabling those teams to prepare for the emergency as they are en route.
Allowing pre-admission registration in motion facilitates quicker patient processing upon arrival.
4. Faster Diagnostic Turnaround
Lab Automation Process Diagnostic of Emergency Patient
These provide real-time access to test results for attending physicians in connected imaging and pathology systems.
Point-of-care diagnostic devices minimize reliance on centralized laboratories, enabling tests to be conducted on-command.
Fixing the Crisis of Emergency Department Delays: What Needs to Be Done
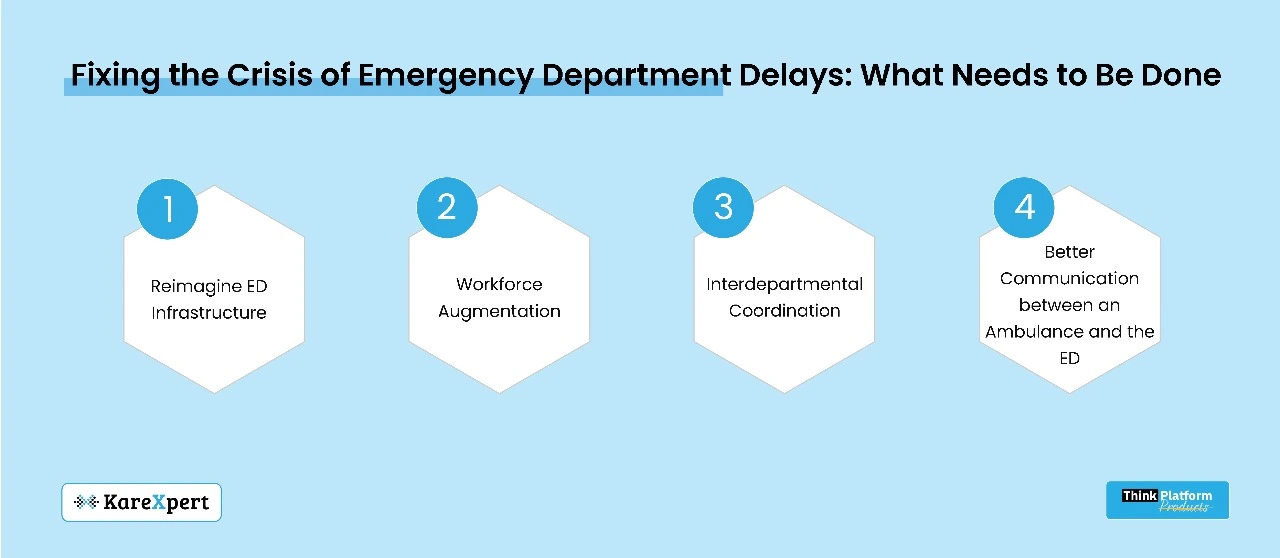
1. Reimagine ED Infrastructure
The plan should create “fast-track” zones for cases in urgent need of treatment but care that does not require ICU levels of intervention.
Smart queue management systems are capable of categorizing patients into critical, urgent, and non-urgent streams.
Specialists in dedicated triage units can ease the burden on beleaguered ED staff by off-loading less serious cases.
2. Workforce Augmentation
Real-time shift optimization tools ensure the right number of staff is working at each time through peak hours.
Automating administrative tasks with AI-powered virtual assistants helps alleviate nurse workload.
Programs providing mental health support to emergency staff can mitigate burnout and increase retention rates.
3. Interdepartmental Coordination
ED, inpatient, and surgical departments all work together seamlessly to advance treatment plans and expedite procedures.
Common digital health records (EHRs) guarantee that treating physicians can instantly review complete patient histories.
Automated discharge planning allows to free up beds in a timely manner, optimizing patient flow.
4. Better Communication between an Ambulance and the ED
Pre-hospital care coordination enables paramedics to relay patient vitals before they reach the scene.
AI-Powered Predictive Tools Predict ED Congestion and Redirect Ambulances to Less Crowded Facilities
Voice-to-text documentation enables paramedics to forward immediate case summaries to the ED, reducing reporting delays.
Conclusion: Real-Time Action Is the Key to Future Emergency Care
If hospitals are still using 1980s workflows, emergency departments will live in a constant state of emergency. The future of emergency care will need to leverage real-time data, AI-driven triage, automated logistics, and predictive analytics in order to stay ahead.
The objective is far from complicated: Quicker interventions, enhanced patient outcomes, and streamlined emergency systems. The answer is simple: The need for digital transformation is not just a choice but a compulsion.
The question is, are you hospital prepared to keep pace with future emergency care?
