Digital Burnout in Hospitals: Are Your Clinicians Drowning in Software?

Introduction: A New Type of Exhaustion
Walk through any modern hospital, and you will find clinicians engaging with screens as much as with patients. Tablets in hand, switching back and forth between dashboards, updating electronic records, answering alerts, clicking through menus, logging into systems. Healthcare has never been so digitized. But for many, this transition has quietly ushered in a new brand of fatigue: digital burnout.
It’s not just about being physically tired anymore. The problem is cognitive overload, decision fatigue and emotional toll created by poorly designed, overly complex, fragmented digital systems. These tools were designed to alleviate some of the burden and better the care, but they instead present another level of complication for the doctors and nurses to work through.
This article examines why digital burnout is being called a crisis in silence in hospitals, and what healthcare leaders can do to reverse it.
The Daily Digital Treadmill
Patient care should be the focus on a typical day in a hospital. But more and more it’s about interfaces. Clinicians spend hours documenting care, reviewing patient histories, ordering labs, logging medication, reconciling data — across multiple software solutions that seldom talk to each other.
Each task is a click, every click is a micro-decision, and every micro-decision is mental fatigue. Doctors say they spend more time interacting with screens than with patients. Single username and password for everything is gone, and nurses log in to multiple applications with several splash screens between disconnected modules.
And unlike the kind of physical fatigue that comes from a long shift, digital burnout seeps in slowly. It starts as frustration, mutates into disengagement and, potentially, blossoms into clinical errors, absenteeism or outright attrition.
Why Are We Here?
So here’s a look at some of the culprits that underpin this digital distress:
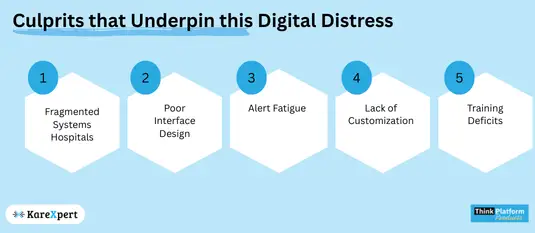
– Fragmented Systems Hospitals buy systems in silos: one for billing, one for radiology, one for EMRs. Clinicians must then toggle between many platforms, none of which give a cohesive picture over time. This patchwork is time-consuming to reorganize and add on to, and leads to an ever-greater risk of mistakes.
– Poor Interface Design Most healthcare software is built with compliance and admin-first workflows instead of clinical logic. User interface is not really intuitive, many clicks, redundant data entry, unergonomic design.
– Alert Fatigue The unending stream of pop-up alerts, reminders and notifications — most low priority — causes clinicians to stop taking notice of even the high-priority alerts. People eventually stop listening.
– Lack of Customization Each department does things in its own way. But for many systems, adaptive capabilities to specialty-specific workflows are limited. This one-size-fits-all approach compels clinicians to navigate the system instead of partnering with it.
– Training Deficits Users are not effectively prepared by a rushed implementation or no onboarding. When the tools of the digital office become painful instead of helpful, morale sinks.
The Price of Not Addressing Digital Burnout
Burnout doesn’t spare clinicians, either. It sends shock waves through the entire ecosystem:
– Patient Safety: We make errors when we’re fatigued. Burnout is associated with increased risk of diagnostic errors, missed information, and incorrect documentation.
– Operational Efficiency: If clinicians are bogged down by tech, they end up slowing down workflows, delaying patient discharges and aggravating bottlenecks.
– Attrition and Recruitment: Nobody wants to work in an environment where the tech makes their jobs more difficult. Skilled employees are expensive and time-consuming to replace.
– Tangible Human Costs: Responsibilities fall through the cracks, rework leads to overtime and mistakes, causing the costs of doing business to rise.
The Early Signs of Digital Burnout in Clinicians
– Inadequate usability of the system as per frequently received complaints
– Less face-time with patients
– More “pajama time” on documentation
– Fatigue and negligence of alerts
– Avoidance of system features
– Becoming disengaged or distant
Restoring the Experience: Putting People Before Technology in Digital Health
These digital tools are not bad in and of themselves. The issue is not with the tools but how they are created and felt. A well-designed system should alleviate friction, not increase it.
Here’s how healthcare executives can reimagine the digital experience:
1. Involve Clinicians in Design Never purchase or develop systems in boardrooms. Get real users doctors, nurses, technicians — involved in the design and selection process. Obtain input continuously and keep it in a cycle.
2. Make Workflow Integration a Top Priority Select integrated technology platforms that bring together disparate modules under a single interface — from pharmacy and radiology, to patient records and discharge planning. The fewer the logins, the better.
3. Simplify the UI/UX Every second counts. Interfaces need to be neat, logical, and ergonomically matched to the needs of clinicians. Minimize clicks, declutter, and automate wherever possible.
4. Rationalize Alerts Institute an alert system with tiers, graded by severity. Reduce noise. Make sure when an alert comes up that it counts.
5. Offer Customization Enable departments and users to tailor dashboards and templates to their day-to-day requirements. Let orthopedic medicine be its own thing — not pediatrics.
6. Invest in Training Digital onboarding should never be a one-time event. Provide ongoing workshops, tutorials, and peer-support groups. Adoption should be an empowering process, not an unfair one.
7. Monitor Clinician Sentiment Use periodic surveys and system logs to track usage patterns and burnout signals. Leverage data to see where the friction is building and act accordingly.
A New Perspective on Digital Transformation in Hospitals
Digital transformation shouldn’t just be trading one type of burden for another. The aim has to be the reverse: to free. To make work lighter. To open up the tools clinicians need to care, not click.
Digital systems in hospitals need to be seen from a human perspective. Clinicians are not data-entry clerks. They are healers. Every second they’re wrestling with software is a second they’re away from the patient.
The future is in designing spaces where technology melts away — the means to an end, quietly performant, invisibly present, meaningfully intuitive. The best tech is the stuff you don’t notice.
Conclusion: Time to Do Something About the Flow
Digital health is not the problem. It’s fragmented, over-engineered, consumer-hostile digital health. The clinician’s digital ecosystem can no longer be less supportive than their physical one. It needs to lower cognitive load, not raise it.
Hospitals have the opportunity — and responsibility — to reframe their digital infrastructure from a checkbox to a strategic tool for workforce well-being and patient safety.
If clinicians are software-shark bait, then the waters need a redesign. One click at a time.
